All the manifestations of muscular dystrophy worsens as the muscles continually deteriorates and starts to weaken, and hence, it is considered as a “progressive muscular disorder”.
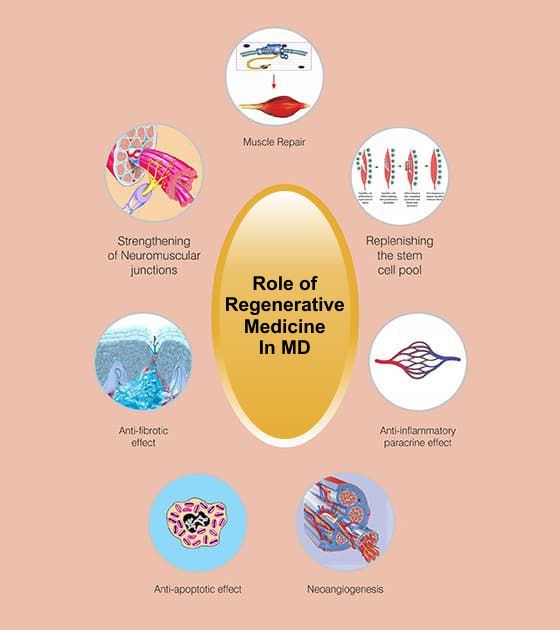
Autologous Bone Marrow Mononuclear Cells Grafting has a promising potential to transmit progressive muscle proteins and restore the stem pool, thus, being the right muscular dystrophy treatment in India approach due to MD’s for deteriorative nature.
bone marrow-derived cells have the capacity to convert into any type of body cell and undergo self regeneration. The capacity of adult muscle to undertake renewal is largely credited to a distinctive subpopulation of muscle cells, called satellite cells. These cells are believed to be the chief cell type associated with skeletal muscle regeneration.
Muscular dystrophy can wear out the emotional, physical and financial condition of the patients, as well as their caregivers. Autologous Bone Marrow Mononuclear Cells Grafting for muscular dystrophy in India at NeuroGen Hospital has come up as a successful treatment option after years of research and study. This is an incredible leap for not just muscular dystrophy treatment in India, but also the world!
STATISTICS OF OVERALL IMPROVEMENTS IN PATIENTS AFTER MUSCULAR DYSTROPHY AUTOLOGOUS BONE MARROW MONONUCLEAR CELLS GRAFTING
90% patients showed symptomatic improvement
After successful muscular dystrophy cell treatment at NeuroGen BSI, our patients have shown marked improvements.
Increased trunk muscle strength
Limb strength on manual muscle testing and balance
Improvements in ambulation
Improved hand function
Increase in stamina
Better trunk balance.
Autologous Bone Marrow Mononuclear Cells Grafting for muscular dystrophy in India, at NeuroGen, not only changes the patients’ clinical symptoms, but also aims to restore and bring to a halt, the muscle wasting that occurs in Muscular dystrophy. This has been demonstrated by the MRI-MSK reports of these patients.
Objective radiological evidence of improvement after autologous bone marrow mononuclear cells grafting for Muscular Dystrophy
Studies around autologous bone marrow mononuclear cells grafting for Muscular Dystrophy in India at NeuroGen have shown that cells from the bone marrow can regenerate and repair damaged muscle cells.
A treatment plan for muscular dystrophy needs to be personalised depending on the intensity and level of impairment, and the progression of symptoms. This personalisation can only be achieved with a thorough evaluation of the patient. However, it is imperative that the following therapies be followed religiously after autologous bone marrow mononuclear cells grafting for muscular dystrophy, for the best possible outcome!
No muscular dystrophy is mainly a hereditary disorder and it is not at all contagious.
It is not always hereditary. Many researchers states that about 1/3 of all boys that suffers from Duchenne/Becker's muscular dystrophy have no such family history.
The most common type of muscular dystrophy is Duchene. Beckers is the second most common MD and limb girdle muscular dystrophy is the third most common form.
The first symptom that you may notice in your child is they tend to start talking and walking late. But many conditions have different signs. Most parents may notice that their child is not running as fast as the other kids. Or the child may also get up from the ground, in a different way, using his hand for support and may have difficulty in climbing stairs.
Muscular dystrophy can be passed on from either of the parents through an affected gene. In myotonic dystrophy, the carrier can be either one of the parents. In limb girdle muscular dystrophy, the transmission could take place through a recessive gene. This means that both parents are carriers, and they both transmit the disease.
Yes, there is a 50% chance of your daughter being the carrier. To ascertain her case, opt for a genetic testing.
If there is a past record of previous child or sibling having this disease/ condition then it is possible through a in-utero diagnosis of DMD. A Chorionic villus sampling or amniocentesis followed by a DNA testing (MLPA) can probably give some answers.
If there is a family history and a reasonable suspicion, then chances are there. But the symptoms cannot be detected unless the child reaches a certain age.
There are no proven records to support that MD occurs only in children. For example facioscapulohumeral, myotonic and limb girdle muscular dystrophy begins later in life .They are slow in development and less severe than the childhood forms.
Few indications like facioscapulohumeral dystrophy, a weak smile or inability to whistle may indicate a beginning. Similarly, in Limb girdle MD weakness of shoulder and hip is seen and in case of Myotonic MD there is an apparent weakness of feet and hands.
Condition where the muscles get enlarged is known as pseudo hypertrophy. It can be replaced with fatty tissues.
The treatment option to help a child with MD to prolong his walking is to make a surgical release of tight or contracted muscle and help him on learning how to stand the very next day. The second option would be serial casting. This would help your child suffering from MD prolong his walking.
To keep the child ambulatory, regular sessions of physiotherapy and exercises would help. Helping them to stand with the help of push knee splints and high boots is very effective. Surgery becomes the best option when the muscles become very tight and are not stretchable at all.
A surgery can help set the joints straight. The best option to opt for when muscles become very tight and are not unstretchable is surgery alone. However, the amount of walking exercise would depend on the muscle strength of the lower limbs.
These therapies help in preventing contractures, keep muscles strong, help in transfer, improve efficiency of functional activities like standing, walking etc.
If exercises are done beyond the patient's’ capability, it can lead to decline in their health. The patient should not get tired or fatigued. Ample time or rest has to be given between exercises.
Swimming is a good form of exercise for the child or patient of muscular dystrophy. Children should be advised to take up swimming lessons from a very early age. It helps to increase endurance, increases muscle strength and good work up for the respiratory and cardiac muscles.
The major cause of death is respiratory muscle weakness that leads to respiratory difficulty. As the muscles weaken, the child develops scoliosis or an abnormal sideways curvature of the spine. The cough reflex gets into a weak position. Patient becomes more prone to chest infection and leads to difficulty in breathing. Cardiac muscle weakness and cardiomyopathy are other major cause of death in muscular dystrophy patients.
The aim of cell therapy for muscular dystrophy in India, at NeuroGen, is to make the muscles stronger and slow down the deterioration of the muscles. If the patient is walking, the goal is to keep them walking. This indirectly could delay respiratory muscle weakness and prevent scoliosis. This could then prolong overall life expectancy, by reducing the chances of respiratory complications.
The biological task of cells is to repair and regenerate damaged cells. Cell therapy for muscular dystrophy in India, at NeuroGen, exploits this function by administering these cells in high concentrations directly in and around the damaged tissue, where they advance its self healing and repair.
No, there are no ethical concerns surrounding adult bone marrow-derived cell treatment research and bone marrow-derived cell treatment for muscular dystrophy. Ethical concerns are mostly occurs through the use of embryonic cells. Our muscular dystrophy bone marrow-derived cell treatment consists of using cells which are taken out from the patient’s own body and it is free from ethical concerns.
No, the treatment is not painful as the cell therapy for muscular dystrophy is done under local anesthesia and mild sedation. There is no major pain or discomfort during or after the procedure.
The whole session of bone marrow-derived cell treatment for muscular dystrophy is safe and till date none of our patients have shown any signs of neurological deterioration. In rare cases, side effects like headache for 3-4 days, neck or back pain, vomiting, mild rash or pain at the area of bone marrow aspirations may arise. Some unexpected medical complications can occur but that is just a possibility.
This may vary from patient to patient. Some patients make a speedy improvement by 3-6 months while in some cases patients take several months or years together to heal after muscular dystrophy bone marrow-derived cell treatment. And there are some patients that show slight improvements even before their discharge
This will depend on the condition of the patient. If the patient shows signs of improvement after the first procedure then a second transplantation may be suggested by a team of experts. The second transplantation can be suggested anytime between 3-6 months of the first cell therapy for muscular dystrophy.
We will have to review the entire dose of medication before coming upon a decision. Generally we do allow the patients to continue their other medication. But it is better to consult a doctor beforehand.
Since cell therapy for muscular dystrophy is a relatively new therapy and not an existing one, it is difficult to say. It will depend on several factors like the age of patient, type of illness, duration of illness and extent of rehabilitation taken after the treatment.
